Your Path to Better Shoulder Mobility
Living with shoulder pain or limited mobility can affect everything from daily tasks to your overall quality of life. Shoulder arthroscopy offers a minimally invasive, highly effective solution for diagnosing and treating a wide range of shoulder conditions. By using small incisions and specialized tools, this procedure minimizes tissue damage and speeds the healing process, helping you regain strength, confidence, and freedom of movement sooner.
For many patients—from active adults to those dealing with chronic shoulder issues—shoulder arthroscopy provides a pathway back to independence. As part of his commitment to world-class orthopedic care, Dr. Max Greig guides patients through each step of the process, from understanding the surgical procedure to navigating the recovery period where regaining mobility becomes the primary goal.
This guide explains how shoulder arthroscopy works, why mobility is essential after surgery, and how proper rehabilitation leads to optimal long-term function.
You might interest in: How to Sleep Comfortably After Knee Surgery
Understanding Shoulder Arthroscopy
What Shoulder Arthroscopy Is and How It Restores Mobility
Shoulder arthroscopy is a minimally invasive surgical technique that allows orthopedic surgeons to view the inside of the shoulder joint and repair damaged tissues through tiny incisions. A thin camera, known as an arthroscope, is inserted into the joint to provide a clear, magnified image on a monitor.
Through additional small incisions, the surgeon uses delicate tools to address injuries or structural problems.
By avoiding the large incisions associated with open surgery, arthroscopy preserves healthy tissue, reduces postoperative pain, and allows for an earlier focus on restoring mobility. Many patients are able to return home the same day, which further supports a smoother recovery process.
Conditions Commonly Treated With Shoulder Arthroscopy
Patients who experience pain, stiffness, clicking, catching, or reduced range of motion often benefit from shoulder arthroscopy. Surgeons commonly use this procedure to treat issues such as rotator cuff tears, labrum tears, shoulder impingement, and biceps tendon problems. In many cases, these conditions interfere directly with mobility, making arthroscopy an important tool for restoring comfort and function.
When a rotator cuff tear prevents smooth lifting or rotation, arthroscopy allows the tendon to be reattached securely to the bone.
Labrum tears, which destabilize the joint, can be repaired or smoothed to restore stability. For patients with impingement syndrome, arthroscopy creates more space within the joint by removing inflamed tissue or bone spurs that restrict movement.
Each of these repairs contributes to a more mobile, functional shoulder by removing sources of pain and restoring proper joint mechanics.
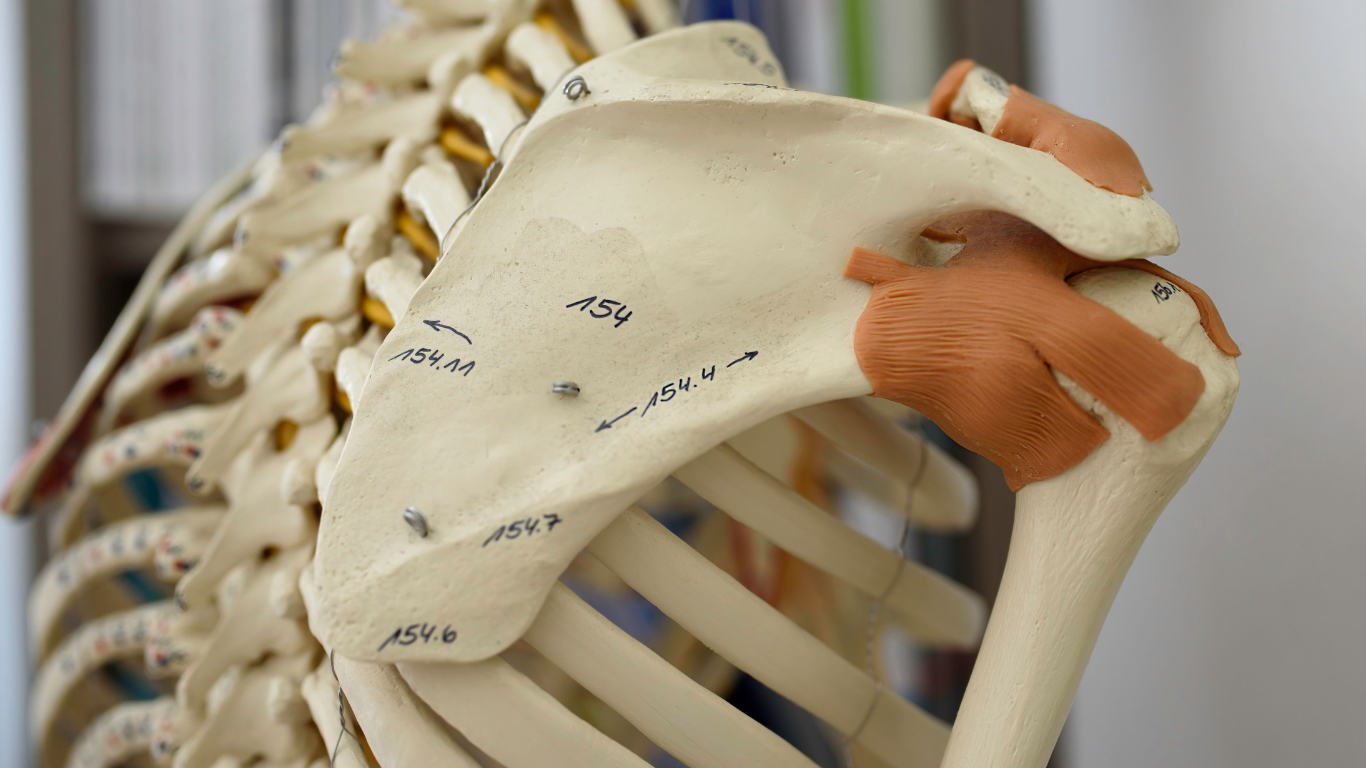
Shoulder Anatomy and Why It Influences Mobility
The shoulder is the most mobile joint in the human body, allowing the arm to move in nearly every direction. This wide range of motion is made possible by the ball-and-socket configuration of the humeral head and the glenoid socket. While this design enables exceptional flexibility, it also makes the shoulder vulnerable to injury and instability.
Healthy shoulder mobility depends on the smooth coordination of bones, tendons, ligaments, cartilage, and surrounding muscles. The rotator cuff tendons ensure stability during movement, the labrum deepens the socket for secure rotation, and the bursa cushions the tissues to reduce friction. When any of these structures are torn or inflamed, shoulder mobility becomes limited or painful.
Shoulder arthroscopy allows surgeons to directly visualize and address these issues with precision. Because the procedure preserves surrounding tissues, patients are able to focus on mobility sooner, which is a crucial factor for a successful recovery.
Minimally Invasive Techniques and Their Benefits for Mobility
Arthroscopy involves inserting a thin camera into the joint and using tiny instruments to perform repairs. This minimally invasive approach reduces trauma to the skin, muscles, and connective tissue. With smaller incisions, the shoulder experiences less swelling and less internal disruption, which contributes to faster healing and earlier movement.
Patients who undergo arthroscopy often begin gentle, supervised mobility exercises earlier than those who have open surgery. Early motion is essential for preventing stiffness, particularly in a joint as complex and prone to tightness as the shoulder. Because recovery begins with less pain and inflammation, patients can progress through rehabilitation more smoothly and safely.
The Importance of Mobility After Shoulder Arthroscopy
Why Mobility Matters During Recovery
Mobility plays a central role in shoulder arthroscopy recovery. When movement is introduced at the right time and in the right way, it helps reduce stiffness, improve circulation, and prevent scar tissue from forming inside the joint. Rest is important in the early days after surgery, but prolonged immobility can lead to long-term limitations.
Gentle, controlled movement not only preserves flexibility but also supports healing by delivering oxygen and nutrients to the recovering tissues. Patients who begin their mobility program on schedule—without rushing—tend to regain a more complete range of motion and experience better functional outcomes.
Benefits of Early Controlled Movement
When mobility begins early and is guided by a trained professional, patients typically notice reduced pain, improved flexibility, and less swelling. Movements such as pendulum exercises or gentle, passive stretching help maintain motion without stressing the repaired tissues.
One of the most significant advantages of early controlled movement is that it prevents the shoulder from tightening or developing adhesive capsulitis (frozen shoulder), a condition characterized by long-lasting stiffness and pain. Maintaining mobility from the beginning significantly reduces the risk of this complication.
Risks of Limited Shoulder Mobility After Surgery
If the shoulder is kept too still for too long, the joint can quickly become stiff. Scar tissue may form inside the capsule, limiting motion in all directions and making everyday activities challenging. Patients may also experience muscle weakness, particularly in the rotator cuff and surrounding stabilizers, which further restricts movement and increases the risk of re-injury.
Limited mobility can also prolong recovery time. A shoulder that becomes stiff early may require additional therapy or even further intervention to fully restore movement. Maintaining regular, guided motion is essential for avoiding these setbacks.
Timeline for Regaining Mobility After Arthroscopy
Recovery progresses gradually and should always follow medical guidance. Most patients begin with passive movement in the first couple of weeks. This means the shoulder is moved gently without using the muscles directly. The goal during this phase is to prevent stiffness while protecting the repair.
Active-assisted movement typically begins between the fourth and eighth week. During this stage, the patient participates more actively in moving the arm, often using the opposite hand or a therapist’s support. This is an important period for regaining flexibility and beginning to rebuild muscle control.
By the third month, many patients move into the active movement phase, using their own strength to raise, rotate, and lift the arm. As the healing progresses, more advanced exercises are introduced to rebuild strength and stability. Full mobility often returns around six months, although more complex repairs may require additional time.
Rehabilitation Strategies for Optimal Mobility
The Role of Physical Therapy
A structured physical therapy program is essential for restoring mobility safely and effectively. In the early stages, your therapist will guide your shoulder through passive motions to prevent stiffness. These controlled movements protect the repair while preserving flexibility.
As you progress, the therapist introduces active and assisted exercises that allow you to use your muscles gradually. Physical therapy typically lasts between six and twelve weeks, although some patients may need additional sessions depending on the type of surgery and their personal goals.
Regular attendance and careful adherence to the therapist’s guidance are crucial. Each session builds on the last, supporting gradual improvements in mobility, strength, and overall shoulder function.
You might interest in: Herniated Disc Surgery Recovery Time: What to Expect After the Procedure
Exercises That Support Mobility and Strength
Exercises vary depending on your phase of recovery, but most rehabilitation programs begin with simple, gentle movements like pendulums or passive overhead raises. These exercises keep the shoulder from tightening and help maintain range of motion.
As mobility improves, strengthening exercises for the shoulder blade and rotator cuff are gradually added. These movements are essential for restoring stability and preventing imbalance. In later stages, resistance bands, light weights, and functional movements help rebuild strength and coordination.
Mobility also relies heavily on consistent stretching. Gentle, daily stretching ensures that the joint continues to open up and move freely. Patients who follow their home exercise program diligently tend to make faster and more complete progress.
Precautions to Ensure a Safe Recovery
Protecting the shoulder in the early stages is essential. Avoid lifting anything heavy, making sudden movements, or reaching overhead without clearance from your healthcare provider. Pain should guide your progress; discomfort is normal, but sharp or increasing pain is a signal to stop.
It is also important to avoid skipping therapy sessions or rushing through exercises. Doing too much too soon can damage healing tissues, while doing too little may lead to stiffness and limited mobility. Finding the right balance is key.
Managing Pain and Swelling to Support Mobility
Pain and swelling can interfere with mobility, so managing them well contributes to smoother progress. Ice therapy is particularly effective and can be used several times a day for short periods to reduce inflammation. Anti-inflammatory medications may also help when approved by your doctor.
Rest is equally important. While mobility is necessary, overusing the shoulder too soon can aggravate pain and delay healing. Elevating the arm, keeping it supported in a sling when instructed, and pacing your daily activities will help control swelling and protect the surgical repair.
You might interest in: Shoulder Surgery for Athletes: Recovery and Return to Sport
Long-Term Mobility and Outcomes
Preventing Stiffness and Future Problems
Maintaining mobility long after the initial recovery phase is essential for protecting shoulder health. Continuing with recommended exercises helps keep the joint flexible and strong. Many patients benefit from incorporating low-impact activities like swimming or walking to maintain overall shoulder and upper-body conditioning.
Avoiding repetitive overhead movements, correcting posture, and maintaining a healthy lifestyle also play a role in preserving long-term mobility. Staying mindful of shoulder mechanics can prevent future injury and ensure the improvements gained from arthroscopy last for years.
Lifestyle Adjustments That Support Shoulder Mobility
Small changes in daily habits can make a significant difference. Improving workspace ergonomics, adjusting sleeping positions, and avoiding movements that place excessive strain on the shoulder all contribute to better joint health. Regular exercise that strengthens the surrounding muscles adds stability, which in turn supports safer motion.
A balanced diet and healthy weight also promote joint health by reducing inflammation and improving overall recovery capacity.
Tracking Your Progress Over Time
Monitoring your mobility and pain levels helps identify areas that need attention. Many patients keep a journal to track improvements in range of motion, strength, and daily function. Follow-up appointments with your surgeon or therapist ensure that your recovery is on track and allow timely adjustments to your rehabilitation program.
If new stiffness or pain arises, addressing it early helps prevent long-term issues. Imaging or additional evaluation may be recommended to ensure that healing is progressing normally.
Frequently Asked Questions
What is the typical recovery time after shoulder arthroscopy?
Recovery varies depending on the type of repair, but most patients experience significant improvement within three to six months. Complex repairs may take longer, especially when tendons need additional time to heal.
When can I begin mobility exercises after surgery?
Most patients begin mobility exercises within the first week, starting with very gentle, passive motions. Your surgeon and therapist will determine the appropriate timing based on your specific procedure.
Is it safe to do cardio exercise during recovery?
Low-impact cardio exercises such as walking or stationary cycling are generally safe early in recovery, as long as they do not involve using the operated arm. Activities that require upper body movement should only be resumed with medical approval.
When can I return to regular workouts or sports?
Many patients return to normal workouts between three and six months after surgery, depending on the demands of the activity and the extent of the repair. High-impact or overhead sports may require clearance and additional strengthening.
Restoring Long-Term Mobility With Expert Orthopedic Guidance
Shoulder arthroscopy is an effective and minimally invasive method for restoring mobility and improving long-term shoulder function. With the proper surgical repair, guided rehabilitation, and a commitment to consistent movement, patients can expect significant improvements in strength, flexibility, and daily comfort.
For individuals seeking experienced, compassionate orthopedic care, Dr. Max Greig offers a unique combination of advanced training, personalized attention, and a patient-centered approach. His guidance throughout the surgical and recovery process ensures that each patient receives the individualized support they need to return to the activities they enjoy with confidence.
Understanding your recovery, embracing your mobility program, and working closely with your care team will help you achieve the best possible results—and reclaim the freedom of movement that supports a healthier, more active life.

.png)


